At Alberta Blue Cross®, we pride ourselves on our approach to drug management. Simply put, we consider the scientific, therapeutic and economic value of drugs to create plans that are sustainable while prioritizing our plan members’ health needs. And because of our expertise in drug management, we field a lot of questions from our clients—plan sponsors large and small.
One category of drug we’re getting questions about is Ozempic.
What is Ozempic?
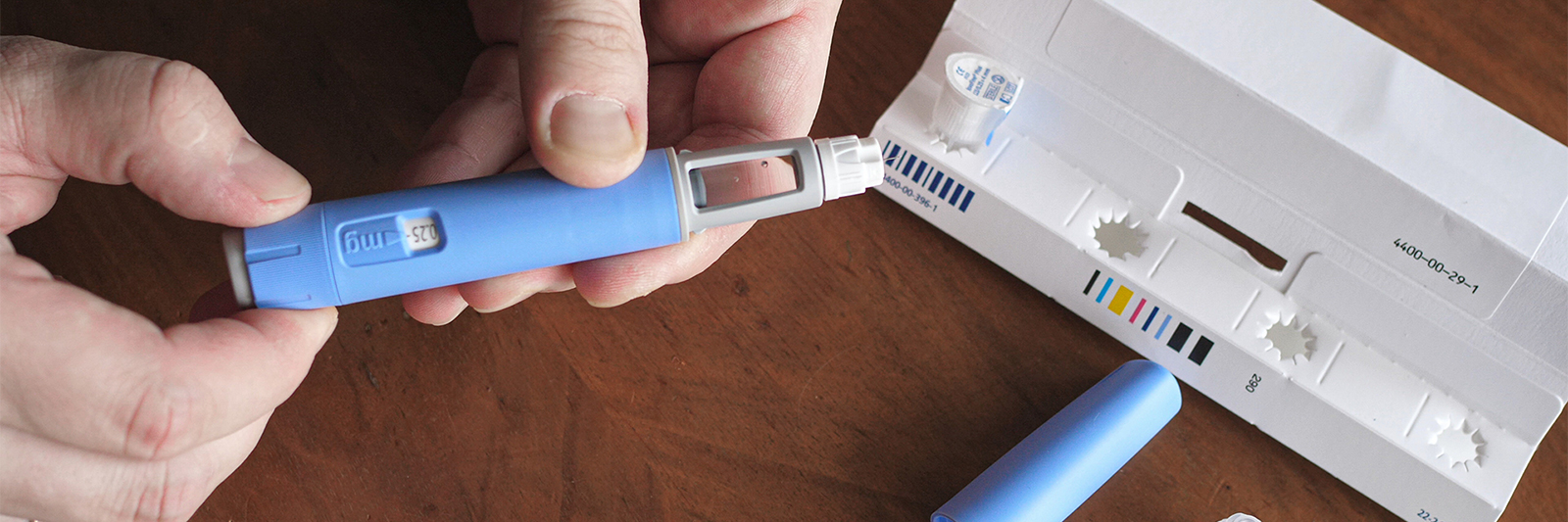
Ozempic is approved by Health Canada as a treatment for adults with Type 2 diabetes. It belongs to a class of drugs called glucagon-like peptide-1 (GLP-1) receptor agonists. This class of medication has been successful in managing diabetes as it lowers blood sugar levels while improving overall blood sugar control.
Why does it seem like everyone’s talking about it?
Ozempic has been featured in the news a lot lately, and not just because of the impact it has on people with Type 2 diabetes. It’s been getting media coverage for a use for which it isn’t approved in Canada: weight loss.
In addition to media coverage, insurers are talking about it as well. The growth in Ozempic use is driving up diabetic drug costs as well as overall costs of drug plans. To ensure Ozempic is being used for its approved purpose, other insurers now need to tighten their management of the drug.
How is Alberta Blue Cross® managing this drug?
From day 1, on our most utilized formulary—our managed formulary—we have been managing Ozempic through our Special Authorization process. Coverage has been, and will continue to be, approved only for use in Type 2 diabetes as per the Health Canada approved indication.
Health Canada provides guidance on prescription drugs as they are Canada’s regulatory body that approves drugs and their indications for use. We therefore align our Special Authorization criteria to a drug’s Health Canada-approved use(s).
If you’re not an Alberta Blue Cross® plan sponsor, you may wish to find out how Ozempic is being managed on your plan.
If plan members are looking for weight loss drugs, what’s available to them?
Chronic obesity was recently designated a chronic disease by the World Health Organization (WHO). It can lead to other serious and costly health conditions including cardiovascular disease, diabetes and even certain types of cancer. In Canada, about 1 in 4 people are living with obesity. In Alberta, our obesity rate is slightly higher at about 28 per cent.
Historically, private drug plans haven’t covered weight loss drugs as it was classified as a ‘lifestyle’ drug category. However, given the recognition of obesity as a chronic health condition with costly co-morbidities, many plan sponsors are looking to update and modernize their drugs plans to include coverage for weight loss drugs.
Currently, weight loss drugs available in Canada include Contrave, Saxenda and Xenical. Wegovy, which contains the same ingredient as Ozempic, but in a higher dose, is also approved in Canada; however, it isn’t available to Canadians yet because of supply issues due to the high demand internationally, particularly in the US.
What do plan sponsors need to know?
At Alberta Blue Cross®, we closely monitor the growing pipeline of new drugs, evaluating their impact on our benefit plans at the earliest stages. This strategy ultimately drove our decision to list Ozempic via Special Authorization on our managed plans, ensuring the best use of drug plan dollars from day 1.
Monitoring drug and health technology pipeline is just one of the many ways we stay up to date on the ever-changing benefits landscape. We are happy to share this expertise to help clients achieve their benefit plan goals.
Questions?
We’re here to help you make the best decisions for your company and your workforce. If you have any questions about this topic or other plan management strategies, please don’t hesitate to contact your Alberta Blue Cross® representative or use the contact form.


my boyfriend put me on his drug plan and you guys messed everything up my name is in your computer but I’m scared to apply for benefits with
Hi there. Please contact us for more information and help with your plan. Our number is 1-800-661-6995.
Why is Ozempic the needle covered but not Ozempic the pill not covered under alberta health. I am a type 2 diabetic and have taken two needles once a week for many years. My side is all blue and black.I am a senior and cannot pay $309 a month for the pill.when will you cover the pill on your pkan
Hi Beverly. Please give our customer service team a call and they will be able to provide you more information about this. 1-800-661-6995. Cheers.
Quite an informative article. Ozempic can help manage a healthy weight, provided patients also practice other healthy habits, such as portion control, physical activities, etc.
As someone who has gone through a radical hysterectomy, and a massive weight gain due to the medical induced menopause, I can tell you for a fact that “portion control & healthier habits” is utter tripe. I find it ludicrous that a plan we’ve paid into for years has taken this stance. I didn’t choose to have cancer, I didn’t choose this weight gain, I was not lazy or unhealthy. This is just another point of frustration on an already garbage situation.
I agree. I gained weight due to a drug I was told would cause weight gain. I did not have a lot of choices, that did not cause weight gain. There are so many factors involved with obesity, which also includes genetics. I’m happy to see when I go to my Doctors office, there are posters on the wall saying there are medical treatments for obesity. 20 years ago, it was the opposite.
Because obesity can lead to other conditions, doesn’t it make more sense for the insurance companies to pay for these medications, which in the long run will save them more money because people will be less likely to suffer from secondary conditions as a result of obesity, one of them being Diabetes?
Wouldn’t it be better to fund these treatments now to prevent having to pay the cost of these medications when patients actually become diabetics?
On the level of each individual’s health status, wouldn’t their overall health and quality of life be better if they had access to medications that could treat obesity now and possibly prevent them from becoming diabetic in the future? Isn’t Prevention worth a pound of cure?
Ozempic will work but watch that you’ll lose muscle mass as well as the visceral fat from your body. Upon my own research, I have come across two good books that may help people fight the good fight against eating sugar, and how the industry has incorporated so much sugar into most of our foods that it feels like an epidemic of obesity. Metabolical by Dr. Robert Lustig and the diabetes code by Dr. Jason Fung, along with their YouTube videos, have helped educate me further and understanding what is happening to our bodies.
I want this post to not just be a comment. I want to offer that shortcut that people may not know about type two diabetes and what I learned to that. It’s a dietary disease not necessarily a hereditary disease and yes it can be reversed. I cannot say that it’s simple, but what is hurting us is sugar, refined, sugar, refined foods, corn, fed animals if you eat meat or fish, but I won’t get into the chemicals that they use also for the green stuff that’s good for us we have to eat sometime. I am trying to offer a shortcut for those that don’t want to do the research I did watch some of those videos. They’re pretty interesting on what Dr. Lustig has to say. Dr. Fung will teach the fasting side of things and how you can get off insulin and other medication’s I’m halfway there. I just need some help in getting my pancreas to release insulin.
Believe it or not insulin is what causes insulin resistance. If you don’t think this is true, why is our intake going up each time you can only cram so much sugar into an insulin cell, then it spills over into your blood. The other issue is fructose your liver can only metabolize this. This will cause the metabolic syndrome and fatty liver and a fatty pancreas but again I’m no professional I shouldn’t be saying this unless it’s been approved by Blue Cross but if everybody can, please look into what the two books have to say it would really help, you get started and educate you better on what’s happening to your body.
I am currently on Ozempic with my current benefits company. When I turn 65 does the coverage automatically continue?
Hi Jan! When AHCIP records indicate an Albertan will be turning 65, a package is mailed to the address on their AHCIP file providing information about programs and services for seniors. This package will include a letter asking you to submit proof-of-age documents if required. If you did not receive the package, or have further questions, contact the AHCIP office: https://www.alberta.ca/ahcip-contact
Hello just a quick question why does blue cross not cover ozempic , when it comes to woman diagnosed with PCOS (polycystic ovarian syndrome)?
Hi Katelyn, for more information about your coverage, please give our customer service team a call at 1-800-661-6995. Thank you!
Will this be changing now that Wegovy is available in Canada? I hear of other insurance companies covering it, so I would like to know why Alberta Blue Cross does not.
If prescribed by my physician for type 2 diabetes, does he need to send confirmation on that for coverage?
Hi Jean, coverage is dependant on your plan. Please give our customer service team a call at 1-800-661-6995 and they will be able to assist you with this.
To Alberta Blue Cross official:
Hello there!
My A1C has been increased to 6.4% through last 3-4 years and i was diagnosed as pre-diabetes last year. I was on Metformin for more than 6 months but wasn’t able to control A1C. so I went on Ozempic without insurance. I just turn 65 last week and my Blue Cross will be in effect on June 1st. Would you please advise if Blue Cross will cover my Ozempic? Thanks!
Hi there. Thanks for reaching out! For more information about the Alberta retirement benefits, please visit https://www.alberta.ca/ahcip-contact
Why are you not covering Wegovy yet?? It has now been approved by Health Canada and obesity is not a “lifestyle”. A healthy weight is crucial for overall health so please start covering this medication.
Now that Health Canada has recognized obesity as a chronic disease, will Blue Cross cover the cost of Ozempic and other GLP-1 medications for those of us that have a prescription from our family physician? When do you anticipate this to happen?
Hi Nancy, coverage is dependent on your plan. Please give our customer service team a call at 1-800-661-6995 and they will be able to assist you.
I would like to reiterate the question stated above: Now that Health Canada has recognized obesity as a chronic disease, will Blue Cross cover the cost of Ozempic and other GLP-1 medications for those of us that have a prescription from our family physician? When do you anticipate this to happen?
However, given the recognition of obesity as a chronic health condition with costly co-morbidities, many plan sponsors are looking to update and
modernize their drugs plans to include coverage for weight loss drugs.
Currently, weight loss drugs available in Canada include Contrave, Saxenda and Xenical. Wegovy, which contains the same ingredient as Ozempic,
but in a higher dose, is also approved in Canada; however, it isn’t available to Canadians yet because of supply issues due to the high demand
internationally, particularly in the US.
How and when is this going to change in order to be proactive in providing necessary assistance in weight management? The difference in daily health that I have seen at taking off 50 lbs is already helpful, but I need to take off at least 50 – 70 lbs more to be considered a “healthy weight”. Unfortunately, at approximately $500 a month, all of my health spending is used up, so I will have to stop in the middle of this treatment unless this will be covered. Related to my weight is chronic joint issues, sleep issues (sleep apnea – directly related to high blood pressure), complications to fibromyalgia muscle pain, breathing issue when trying to exercise. Taking off the weight to a healthy BMI will mean less joint and pain management medications, potential reduction in my Fibromyalgia medications, better sleep, etc, and likely reduction or removal of my 2 blood pressure medications!! By providing medications to assist in taking off excess weight, many long term chronic issues and complications related to these could be avoided.
I hope to hear shortly that your members will be properly provided medications to assist to not only to cover current health issues, but for those that will allow us to age in a more healthy manner – ultimately costing our health system less as we will need less care in our older age as well.
Hi Vicki. Thanks for reaching out. Please give our customer service team a call at 1-800-661-6995 and they will be able to provide you with information regarding the coverage of our plans.
SInce Wegovy is now an approved weight loss drug in Canada, when will Blue Cross be covering it for those who desperately need it to help manage their weight? AS Im sue you are fully aware, obesity creates a whole host of more serious medical conditions, so not covering it for those prescribed it by a Dr makes no medical sense at all. Would love an answer here for all who are asking, not just a comment to call Blue Cross for an “explanation”
Hi Marlene, because coverage for medications is dependent on each person’s plan, we are unable to give an answer here that would apply to everyone. If you want to find out if you have coverage for Wegovy, you will need to speak with our Customer Service team. Please give us a call at 1-800-661-6995 and our team would be happy to assist you!.
Blue cross has done nothing but give me an absolute headache, it’s been a nightmare dealing with this, I’ve been on ozempic for 1.5 years and all of a sudden I’m not being covered for it anymore, what happened to the continuity of care?? How can you guys just stop the coverage of ozempic for something that has worked with lowering my insulin levels and creating a better hormonal balance for me? I’m so furious and frustrated. You’d think that if someone has been on it for a while and had already had coverage under blue cross it would be grandfathered. Clearly you guys don’t care about the well being of the people who pay into benefits in order to get life saving or life changing medications.
Hi Celina, thanks for reaching out. For information regarding your coverage, please give our customer service team a call at 1-800-661-6995. Thank you.
Great insights on Ozempic! I’ve been curious about its benefits and potential side effects, and this article really clarified a lot for me. Thanks for sharing such helpful information!
Thank you for this informative post about Ozempic! I found the details on how it works and its potential benefits really helpful. It’s great to see discussions around modern treatments for diabetes and their accessibility in Alberta. Looking forward to more posts like this!
My wife had a drug plan through a former employer which did include approval for her Saxenda prescription. The plan recently expired and when we called them directly for a private plan, they said that it would not be covered. How does this work? if it is covered on an employers plan then there should also be a personal plan available with the same coverage. (The plan was not through Blue cross). If the WHO considers Obesity as a Chronic disease, then these drugs should be covered to reduce the other High risk health issues related to it.
Thank you for the informative post about Ozempic! It’s great to see a comprehensive overview, especially regarding its benefits and potential side effects. I’m curious about how it compares to other diabetes medications in terms of effectiveness and cost. Looking forward to more insights!
A medical study is currently being done on the benefits of GLP-1s in combination with Biologics and the ability to reduce inflammation markers from autoimmune diseases like Rheumatoid Arthritis, Psoriatic Arthritis (PsA) and Psoriasis. I have PsA, and had been on Saxenda for two years (in combination with Infliximab) – not only did I lose weight, but my CRP dropped from 20+ to under 2. Over the past year and half, I had to stop taking Saxenda due to cost reasons, and my CRP has climbed steadily with the return of my PsA symptoms (and weight, obviously) greatly reducing my ability to move without intense pain and stiffness. Will GLP-1 ever be available for non-diabetic use through Non-Group Coverage?
Hi Tammara, for more information about our coverage, please give our customer service team a call at 1-800-661-6995. Thank you!
This blog post provides such valuable insights about Ozempic! I appreciate the breakdown of how it works and its benefits. It’s great to have clear information about the potential side effects and usage guidelines. Thank you for addressing this important topic!
Great post! I found the information on Ozempic really insightful, especially the details about its benefits and potential side effects. It’s helpful to understand how it can fit into diabetes management. Thanks for sharing!
I have group coverage with my employer and was both shocked and disappointed to have had to pay $263 dollars for my prescription today. After over five years of filling metformin and diabetes supplies prescriptions, apparently I’m not diabetic enough to be covered for this medication. Now I need to schedule another appointment, waste the doctor’s time to fill out a form to justify her professional decision, when she could be treating another patient with an actual medical problem. This article is old and outdated and your policy around this medication needs to change ASAP.
Hi Leanne, we’d be happy to help. Please give us a call at 1-800-661-6995 and someone can assist.